Difference between revisions of "Amisulpride-Zuclopenthixol LA"
From Psychiatrienet
| (2 intermediate revisions by one other user not shown) | |||
| Line 4: | Line 4: | ||
| stop = {{Downslweeks}} | | stop = {{Downslweeks}} | ||
| start = {{StartDepot}} | | start = {{StartDepot}} | ||
| − | |||
| info = {{caveQT}}{{Alternatief}} | | info = {{caveQT}}{{Alternatief}} | ||
| + | | view = Stop10WeeksStartDepot.jpg | ||
}} | }} | ||
Latest revision as of 09:13, 11 February 2010
| ||||||||||||||||||||
| ||||||||||||||||||||
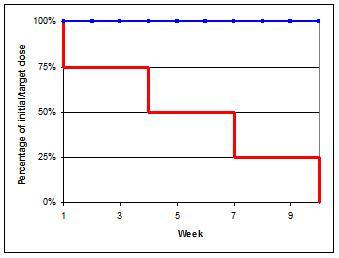
Switch medication from Amisulpride to Zuclopenthixol_LA[1][2]
- Week 1-3: approx. 75% of initial dose
- Week 4-6: approx. 50% of initial dose
- Week 7-9: approx. 25% of initial dose
- Week 10: stop
- Day 1: Start depot according general dosing advice (Dotted line in graph)
- During this switch you could monitor ECG, especially in patients prone to QT-conduction problems.
- There is a possibility of QT interval prolongation.[3]
- Alternatively, first switch to oral form and then switch to depot to manage possible (adverse) reactions. With a direct switch to a depot it is advisable to administer a low testdose in order to exclude adverse reactions.
- ↑ Switches are based on literature references on this page and expert opinions of the authors. The authors have used pharmacokinetic and receptor affinity properties to determine the switch schedules
- ↑ Stahl, S. M. (2013). Stahl's essential psychopharmacology: Neuroscientific basis and practical applications (4th ed.). Cambridge University Press.
- ↑ Stöllberger C, Huber JO, Finsterer J, Antipsychotic drugs and QT prolongation. Int Clin Psychopharmacol. 2005 Sep;20(5):243-51.
The editors of psychiatrienet.nl take the greatest care to provide up-to-date and accurate information on this site. Nevertheless, mistakes and omissions cannot be entirely excluded. No rights devolve from the information provided. The editors and other providers of information to this site accept no responsibility for the content of this site or for the information provided therein; neither do they accept responsibility for possible damages which may derive from the use of the information on this site or from the linked sites. The editorial board accepts no responsibility for the content of the (linked) sites, for access to them, or for the products and services on these sites, nor for the occurrence of errors, viruses, and/or disruptions in service.